Understanding the Link Between PCOS and Period Pain

Polycystic ovary syndrome (PCOS) is a condition that affects women of reproductive age and is characterised by hormonal imbalance, which can lead to a variety of symptoms, including irregular menstrual cycles, infertility, weight gain, and excessive hair growth.
Importantly, PCOS is also associated with dysmenorrhea, commonly known as period pain, which can significantly impact a woman's quality of life. This article delves into the connection between PCOS and period pain, exploring the underlying causes and possible management strategies to alleviate the discomfort associated with this common endocrine disorder.
Introduction to PCOS and Endometriosis
Polycystic Ovary Syndrome (PCOS) and endometriosis are two distinct yet commonly occurring health conditions among women, each with its set of challenges. As individuals navigate their health concerns, questions often arise regarding the possibility of coexisting PCOS and endometriosis. This introduction aims to shed light on the intricacies of these conditions and the importance of recognising their potential coexistence.
Can You Have PCOS and Endometriosis?
The co-occurrence of PCOS and endometriosis is not uncommon, and individuals may find themselves grappling with symptoms of both conditions simultaneously. Understanding this potential overlap is crucial for a comprehensive understanding of one's health. The intricate nature of these disorders necessitates a nuanced exploration to distinguish their symptoms and devise tailored treatment plans.
Exploring the Coexistence of PCOS and Endometriosis
The convergence of PCOS and endometriosis introduces a unique set of challenges, both in terms of diagnosis and management. This section delves into the commonalities in symptoms, such as pelvic pain, irregular menstrual cycles, and hormonal imbalances. By unraveling these shared features, individuals and healthcare professionals can adopt a more holistic approach to healthcare.
Understanding how PCOS and endometriosis intersect provides valuable insights for developing personalised treatment strategies. For instance, addressing hormonal imbalances common in both conditions may require a multifaceted approach.
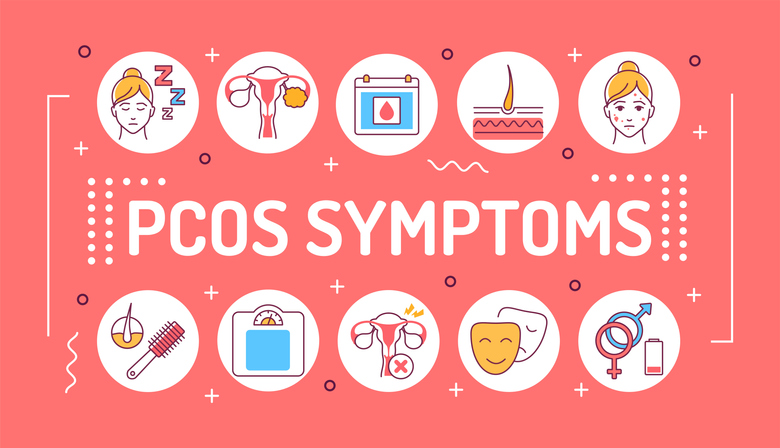
Symptoms of PCOS and Impact on Menstrual Health
Polycystic Ovary Syndrome (PCOS) casts a profound influence on menstrual health, manifesting in various ways that can significantly impact the daily lives of individuals. This section aims to delve deeper into the multifaceted relationship between PCOS and menstrual disorders, shedding light on the causes and management of painful periods and cramps associated with this condition.
PCOS Painful Periods: Causes and Management
Painful periods, medically known as dysmenorrhea, are a common symptom experienced by individuals with PCOS. The root causes of this discomfort are intricate, involving heightened uterine contractions, inflammatory responses, and the presence of ovarian cysts. The overproduction of androgens, often seen in PCOS, contributes to these physiological changes, amplifying the intensity of menstrual pain.
Management strategies for PCOS painful periods related are multifaceted. Hormonal birth control emerges as aprimary intervention, playing a pivotal role in regulating the menstrual cycle. By stabilising hormonal fluctuations, contraceptives contribute to smoother, less painful periods.
Understanding PCOS Cramps and How to Alleviate Them
Cramps during PCOS extend beyond mere discomfort; they can significantly interrupt daily activities and diminish the overall quality of life. The causes of these cramps are intertwined with the underlying hormonal imbalances characteristic of PCOS. Increased androgens and irregular menstrual cycles contribute to the severity of cramps, making their management a crucial aspect of PCOS care.
Alleviating PCOS cramps related involves a comprehensive approach. Hormonal therapy, similar to its role in managing painful periods, plays a central role. By regulating hormonal fluctuations, this therapy aims to mitigate the intensity and duration of cramps. Diet modifications, focusing on anti-inflammatory foods and adequate hydration, can contribute to reducing cramp severity. Incorporating regular exercise into one's routine is another beneficial aspect, as physical activity can alleviate cramps and improve overall well-being.
Can PCOS Cause Bleeding During Intercourse?
The question of whether PCOS can cause bleeding during intercourse is a nuanced one. While PCOS doesn't directly lead to this issue, the intricate web of symptoms associated with the condition may play a role indirectly. Hormonal imbalances, a hallmark of PCOS, can impact the delicate balance of reproductive health, potentially causing cervical inflammation or dryness. These factors, combined with the heightened sensitivity of the genital area, may contribute to discomfort or bleeding during intercourse for some individuals with PCOS.
Connection Between PCOS and Fatigue
While PCOS is often associated with more visible symptoms such as irregular periods and hormonal fluctuations, fatigue quietly emerges as a less-discussed yet equally challenging aspect of the condition. The roots of fatigue in PCOS are complex and multifaceted. Hormonal imbalances, a central feature of PCOS, can disrupt the body's natural rhythms, leading to persistent tiredness.
Does PCOS Make You Tired? Unraveling the Fatigue Factor
Polycystic Ovary Syndrome (PCOS) often introduces a range of challenges, including persistent fatigue and various forms of pain. This section aims to delve into effective strategies for coping with PCOS-induced pain, offering a holistic approach that encompasses lifestyle interventions, supportive therapies, and medical options.
Addressing Tiredness in PCOS: Tips for Management
The chronic nature of PCOS can take a toll on both physical and emotional well-being, resulting in persistent fatigue. To effectively manage tiredness in PCOS, individuals can embrace a multifaceted approach. Regular physical activity plays a crucial role, promoting overall health and boosting energy levels. Prioritising quality sleep is equally important, with strategies such as maintaining a consistent sleep schedule and creating a conducive sleep environment. Stress reduction techniques, including mindfulness and relaxation exercises, can further alleviate the mental fatigue associated with PCOS. Ensuring a well-balanced diet rich in essential nutrients supports sustained energy levels throughout the day.

Managing Pain in PCOS:
Managing Pain in PCOS requires a comprehensive strategy that combines pharmaceutical approaches with lifestyle interventions. Pharmaceutical options may include prescribed painkillers and hormonal contraceptives to regulate menstrual cycles and reduce pain intensity.
Strategies for Coping with PCOS-Induced Pain: A Comprehensive Guide
Coping with PCOS-induced pain involves a personalised approach, considering the unique combination of symptoms each individual may experience. Lifestyle interventions, such as maintaining a healthy weight and adopting an anti-inflammatory diet, contribute to overall well-being and may reduce pain severity.
Abdominal Pain and PCOS: Understanding the Roots
Abdominal pain in PCOS can arise from various factors, including enlarged ovaries, the presence of ovarian cysts, or hormonal fluctuations. Understanding the specific roots of abdominal pain is crucial for tailoring effective treatments. Management may involve addressing hormonal imbalances through medication, lifestyle adjustments to reduce inflammation, and monitoring ovarian health through regular check-ups.
Bilateral PCOS: Comprehensive Treatment Approaches
Bilateral PCOS, impacting both ovaries, can intensify the typical symptoms of the syndrome, including menstrual pain. Managing bilateral PCOS requires a comprehensive treatment plan that addresses multiple symptoms concurrently. This may involve a combination of hormonal regulation, lifestyle adjustments, and targeted interventions to alleviate pain and enhance overall well-being.
Effects of PCOS on Menstrual Health
PCOS significantly influences menstrual health by disrupting hormonal balance. Understanding these effects is crucial for managing irregular menstrual cycles, heavy bleeding, and painful periods associated with PCOS. Tailored interventions, such as hormonal medications and lifestyle adjustments, can help regulate menstrual health and mitigate the impact of PCOS on this aspect of well-being.
Can PCOS Cause Heavy and Painful Periods?
The link between PCOS and heavy, painful periods is rooted in hormonal imbalances that lead to the buildup of the uterine lining. Shedding this lining during menstruation can result in more significant pain and bleeding. Exploring this connection allows for targeted interventions, including hormonal regulation and lifestyle modifications, to address the
specific challenges posed by heavy and painful periods in PCOS.
PCOS and Menstrual Pain: Insights and Solutions
Insights into the physiology of PCOS provide a foundation for developing solutions to menstrual pain. Addressing hormone regulation, managing insulin levels, and considering surgical options, such as ovarian drilling, can offer targeted solutions for individuals experiencing menstrual pain in the
context of PCOS.
Dealing with Period Pain and PCOS:
Effective strategies for dealing with period pain PCOS encompass both medical and non-medical avenues. Adopting a balanced diet, engaging in regular exercise, and possibly exploring complementary therapies contribute to a holistic approach to managing period pain. By integrating these strategies, individuals with PCOS can enhance their
ability to cope with and alleviate the challenges posed by PCOS menstrual pain.

PCOS and Reproductive Health"
Can PCOS Cause Weight Gain and Lead to Infertility?
Polycystic Ovary Syndrome (PCOS) is often associated with weight gain and infertility, posing significant challenges for those affected. The intricate connections between PCOS, weight management, and fertility are crucial considerations for individuals planning a family or dealing with weight-related issues.
Metformin and PCOS: Exploring the Link with Period Pain
Metformin and PCOS, a commonly prescribed medication for PCOS, has implications beyond insulin regulation, including its potential impact on period pain. This exploration delves into the link between metformin use and the management of PCOS symptoms, particularly period pain. Investigating the broader context of metformin use provides individuals with PCOS a comprehensive understanding, enabling them to make informed decisions about their treatment plans and seek relief from associated symptoms.
Teenage Hormone Imbalance and PCOS
PCOS can manifest during adolescence, contributing to hormonal imbalances that may have lasting effects. Recognising the signs and symptoms of PCOS during the teenage years is crucial for early intervention.
Adolescent PCOS: Addressing PCOS Painful Periods and Symptoms
Addressing the unique challenges faced by adolescents with PCOS involves a combination of medical guidance, lifestyle adjustments, and emotional support. This section provides insights into managing PCOS painful periods and other symptoms in the adolescent population.



Leave a comment